Here’s where L.A. County is seeing COVID outbreaks this summer

[ad_1]
Higher rates of coronavirus transmission are leading to more COVID-19 outbreaks in Los Angeles County, with nursing homes, schools and worksites reporting increases in recent weeks.
There were 35 new COVID-19 outbreak investigations among nursing homes in L.A. County for the week that ended Aug. 26, an unusually high number.
“There have only been a few times in the past year and a half when we saw this many new outbreaks in skilled nursing facilities. And these were during the previous summer and winter surges,” L.A. County Public Health Director Barbara Ferrer said at a briefing Thursday.
At schools and other educational settings, there were 27 new investigations for the same week, Ferrer said, similar to what was reported after last year’s summer break and following major school holidays.
“We know that schools are especially susceptible to outbreaks due to the large number of people who are indoors together for an extended period of time,” Ferrer said. “While this increase is not unexpected, since students and staff just returned from summer break, it is noteworthy because it means that COVID is still capable of causing disruptions at schools.”
Parents should keep children at home when they’re sick, Ferrer said.
The number of workplaces reporting new COVID outbreak investigations is also up, with nearly 20 for the most recent week available, up from fewer than five a week earlier. The California Department of Occupational Safety and Health, or Cal/OSHA, requires masking temporarily in workplaces when there is a COVID-19 outbreak.
The L.A. County Department of Public Health also issues temporary mask orders in COVID outbreak settings like work sites if it seems there’s a lot of spread, Ferrer said. The orders usually last until officials stop seeing new coronavirus cases, and they’re typically limited to specific areas where spread has been occurring.
“If you’re in a business that has, like, multiple stories, we don’t tell everybody on every floor to mask,” Ferrer said; the order would focus only on floors where “there’s been a fair number of cases.”
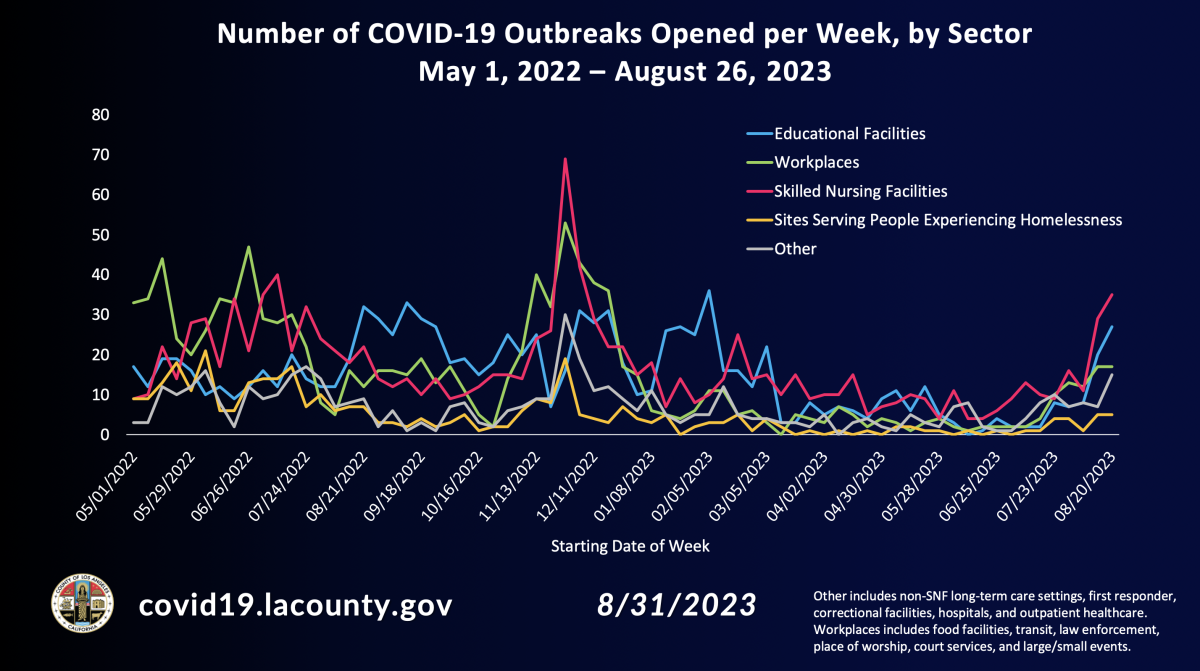
The number of COVID-19 outbreak investigations opened by week in Los Angeles County.
(L.A. County Department of Public Health)
A number of work sites in the entertainment industry have experienced outbreaks recently, including the Directors Guild of America in Los Angeles, “The Masked Singer” studio at Red Studios Hollywood, Lionsgate Entertainment in Santa Monica and Walt Disney Feature Animation in Burbank, according to the county Department of Public Health.
Hospitalizations are rising as well. For the week that ended Saturday, there were, on average, 521 coronavirus-positive patients in L.A. County’s hospitals, about double the level from early August. Still, the latest numbers are less than half of the peaks seen last winter and last summer.
“In fact, there are only four other periods during the entire pandemic when hospitalizations are lower than what we’re reporting this week — and one included earlier this summer,” Ferrer said.
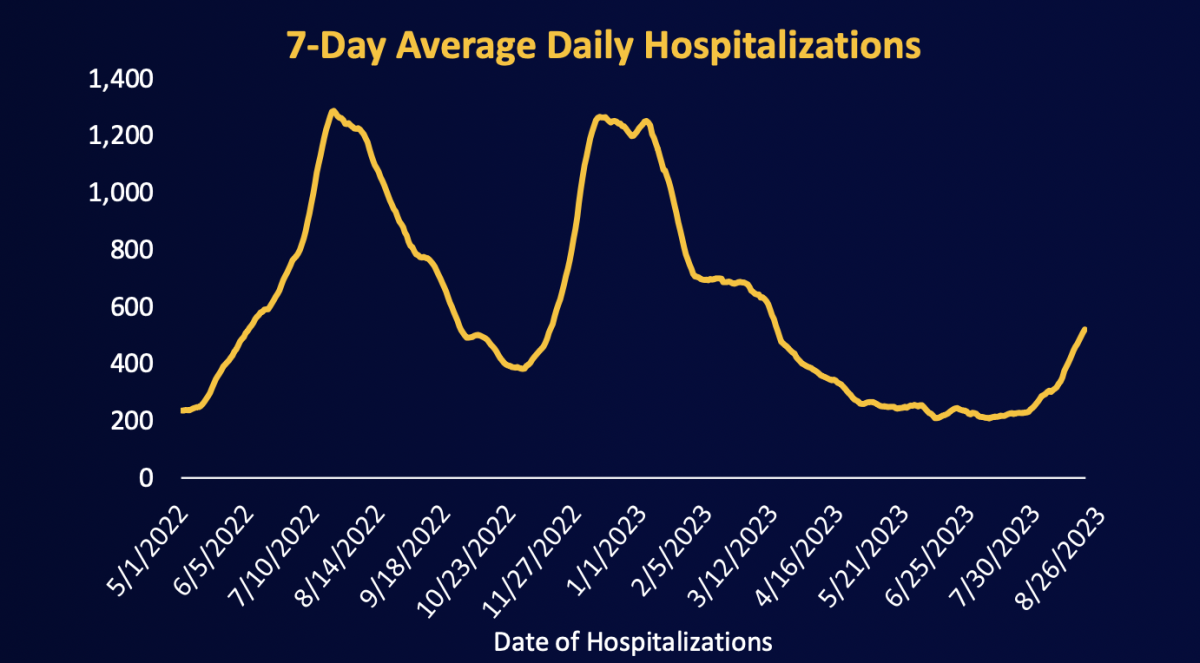
The average number of people in hospitals in L.A. County infected with the coronavirus is up, but still well below last winter’s peak.
(L.A. County Department of Public Health)
The percentage of emergency room visits linked to COVID-19 has increased slightly, Ferrer said. Currently, about 5% of emergency department visits were related to COVID; four weeks earlier, it was 3%.
Despite the increase in coronavirus transmission, there hasn’t yet been a corresponding increase in COVID-19 deaths, which remain at one per day in L.A. County. Rising infections could lead to an increase in deaths, but Ferrer said it’s also possible that deaths could remain low, which “could reflect reduced risk of dying associated with higher rates of vaccination and the use of powerful therapeutics” such as Paxlovid.
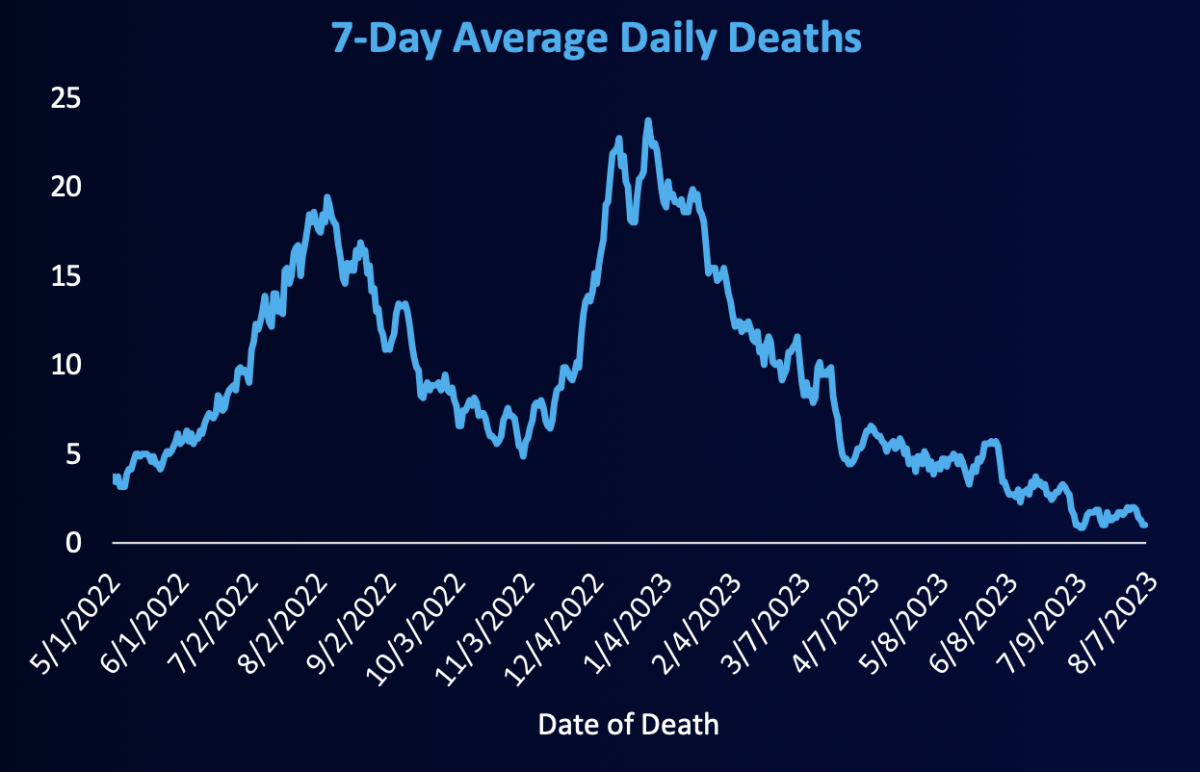
The average number of COVID-19 deaths per day in L.A. County has not climbed in recent weeks.
(L.A. County Department of Public Health)
The proportion of COVID deaths in L.A. County is half what it was this time last year, when the illness was implicated in almost 5% of all deaths, Ferrer said. For the most recent week available, COVID-19 was responsible for about 2.5% of all deaths; for each of the prior two weeks, it was linked to 1% of all deaths.
“It is possible that this could be an early indicator that, maybe, we’re going to see some increased numbers of deaths. Yet, with only one week of data, it’s too early to determine if this is a trend,” Ferrer said. During the peak of last summer’s COVID-19 surge, 7% of all L.A. County deaths were associated with COVID-19.
Although the number of outbreaks at nursing homes is high, they so far have been associated with fewer resident deaths than last year, Ferrer said.
“And this likely reflects high rates of vaccination: 75% of residents in skilled nursing facilities received the bivalent booster and [have] good access to therapeutics,” Ferrer said.
Coronavirus levels also are rising in L.A. County wastewater, but still nowhere near last winter’s surge. For the most recent data available, levels for most of the county’s sewage were at 26% of last winter’s peak. That’s an increase from early July, where viral concentrations in wastewater were at just 8% of the winter peak.
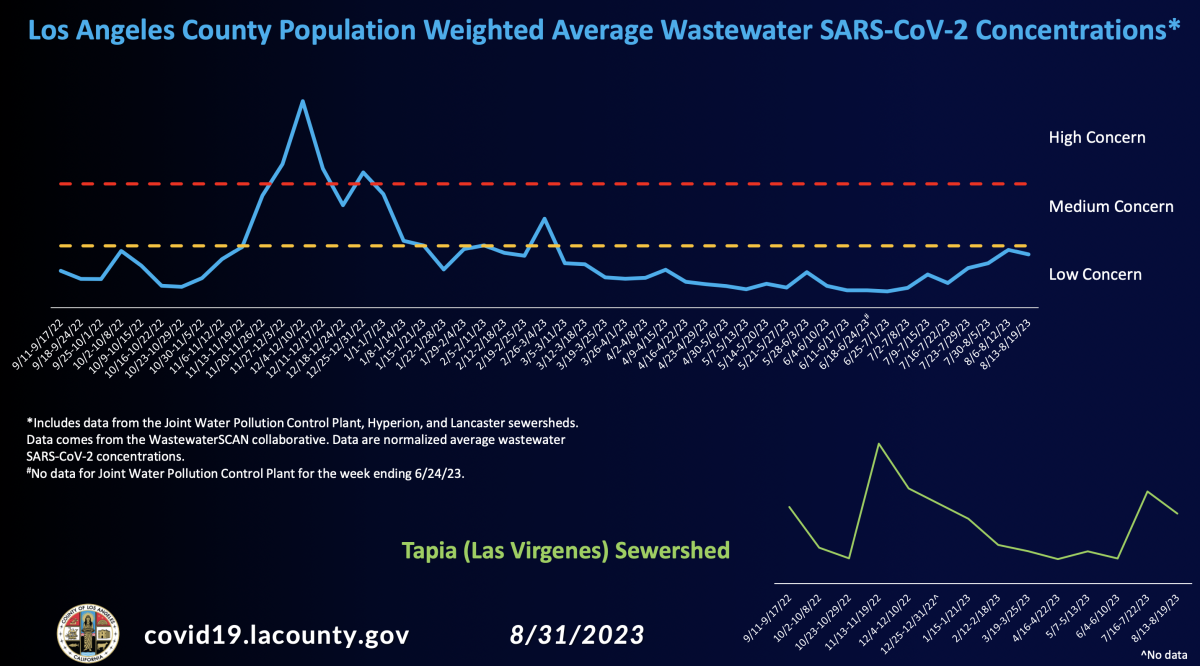
Coronavirus levels in L.A. County wastewater have risen in recent weeks, but still remain well below last winter’s peak.
(L.A. County Department of Public Health)
In L.A. County, the most dominant subvariant is EG.5, also known as Eris, which comprised 21.5% of viral specimens for the week that ended Aug. 5. It’s closely related to the second-most dominant subvariant, XBB.1.5, also known as Kraken, which accounts for nearly 14% of specimens. Both are strains of the Omicron variant.
A new version of the COVID-19 vaccine expected to be available by mid-September is designed specifically against Kraken and is likely to be quite effective against other closely related subvariants, such as Eris.
But officials are closely monitoring another subvariant, BA.2.86, nicknamed Pirola. It has an astonishing 35 new mutations compared with XBB.1.5, Ferrer said, and “it is thought that because of the large number of mutations, BA.2.86 may be more capable of causing infection in people who previously had COVID or who received the COVID-19 vaccines.”
Only 25 cases of Pirola have been identified across eight nations, Ferrer said, including four cases in the U.S. There have not been any cases of Pirola in California, “and at this point, there is no evidence that this strain is causing more severe illness.”
With Labor Day around the corner, Ferrer said the decision to mask can still generally be made based on personal preference. But “given higher rates of transmission, this would be a good time to put your mask on — [a] well-fitting, high-filtration mask — when you’re on public transit and when you’re in healthcare settings,” Ferrer said.
Masking in indoor public spaces still remains prudent for people with an increased risk for severe illness from COVID-19 and those who live or work with them, or anyone who wants to take extra measures to avoid getting sick, Ferrer said.
“Masking when you’re in indoor spaces with lots of people — and/or there’s poor ventilation — will offer you additional protection, even if everyone else in that space is not wearing a mask,” Ferrer said. “And it may be a good idea, if you’re at higher risk for severe illness, to ask folks visiting with you to test for COVID.”
Ferrer said there may be increases in coronavirus transmission associated with Labor Day, “but we’re hoping … that it will be a small bump.” Over the Fourth of July holiday, there was only a “very small” increase in COVID-19 levels, she said.
Ferrer encouraged people to make plans to get the new COVID-19 vaccine when it becomes available by mid-September. Insured people will be able to get the vaccine at no cost, and uninsured children will be able to get the vaccine for free through the federal Vaccines for Children program.
Uninsured adults can get free COVID vaccinations through certain health clinics and pharmacies, as well as the county Department of Public Health. L.A. County will publish a list of locations as soon as it’s available.
[ad_2]